Pain
Arthritis
Symptoms
The symptoms of arthritis include joint pain, stiffness, swelling, redness, and decreased range of motion.
Causes
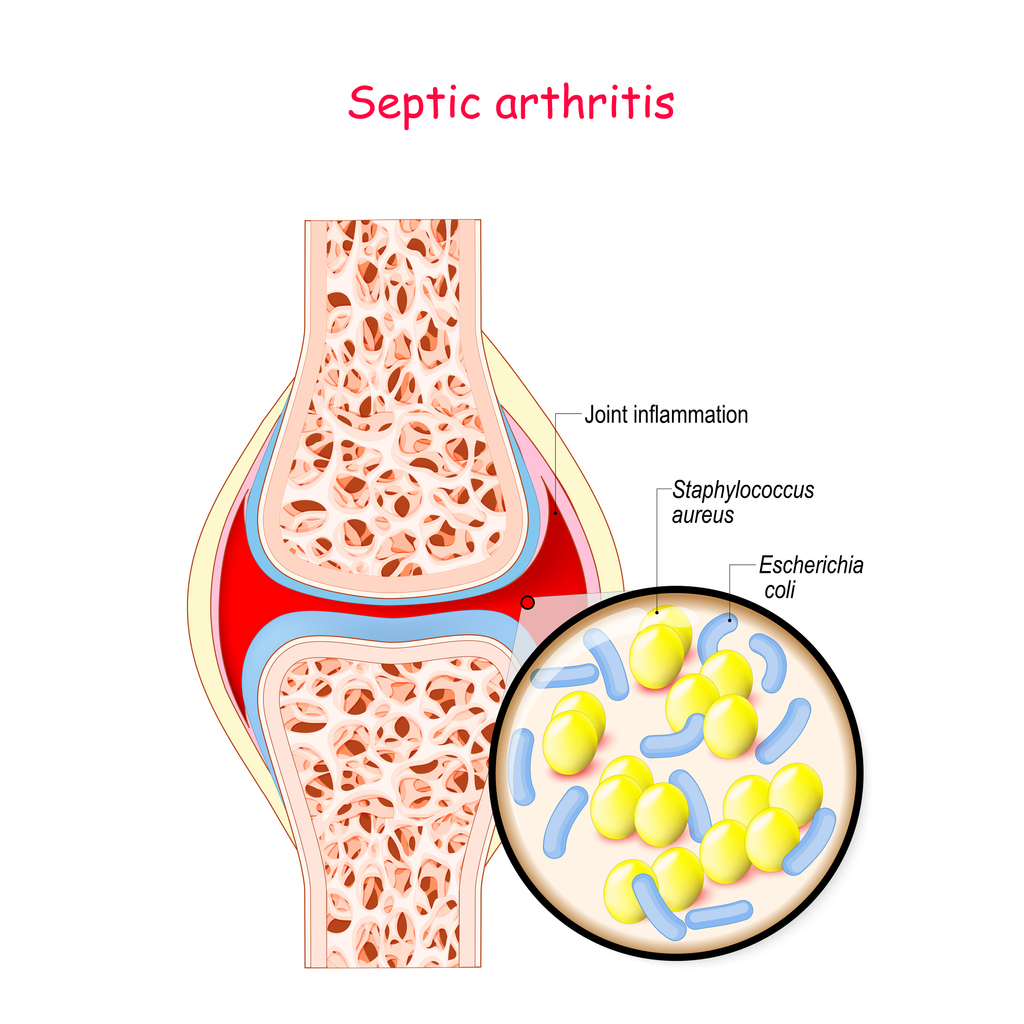
The most common forms of arthritis are osteoarthritis, rheumatoid arthritis, and psoriatic arthritis. Most common causes of arthritis may include injury (leads to degenerative arthritis), abnormal metabolism (leads to gout), inheritance (leads to osteoarthritis), infections (arthritis of Lyme Disease), and immune system dysfunction (rheumatoid arthritis).
Osteoarthritis
Osteoarthritis is a result of worn down cartilage that stops protecting bones rubbing together and causing joint swelling, stiffness, and pain.
Rheumatoid Arthritis
Rheumatoid arthritis causes the body’s immune system to attack the lining of the joint capsule that protects the joint parts. The inflammation and swelling causes pain and eventually destroys the cartilage and bone.
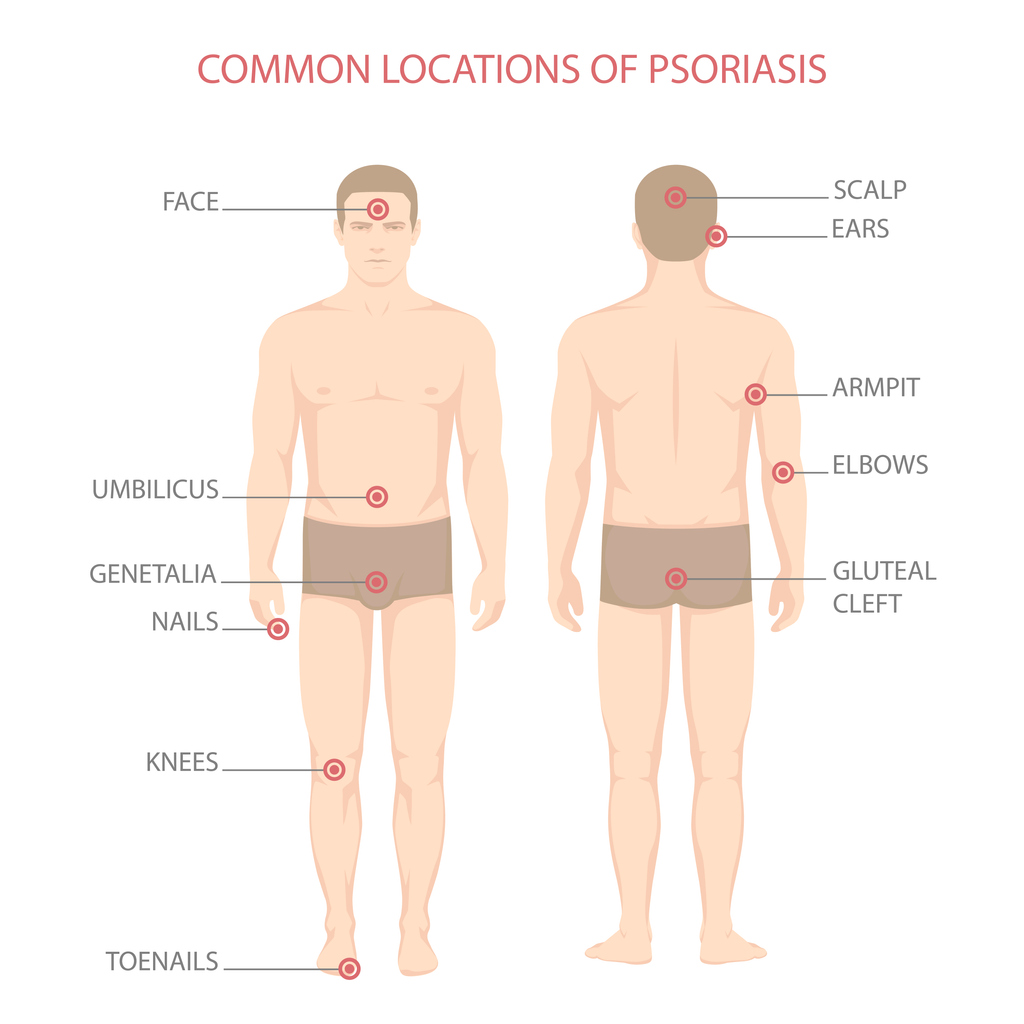
Psoriatic Arthritis
Psoriatic arthritis can accompany psoriasis, a skin disease that creates patches of scaly, red, and white skin. The condition often occurs in the spine (Spondylitis), lower extremities, fingers, toes, and pelvis.
Treatments
Patients have a variety of treatments to choose from including self care, medications therapies, and surgery.
Self Care
Stretching, walking or swimming can help patients improve their flexibility, strengthen muscles, and protect joints from further damage. Managing stress with meditation, yoga, and music can also help reduce the perception of chronic pain. For some patients, dietary supplements (glucosamine) may help reduce arthritic pain.
Medications
Patients can take over-the-counter (OTC) analgesics (Tylenol) or anti-inflammatory medications (ibuprofen or naproxen) to reduce mild to moderate pain. Topical creams that contain mint (menthol) or pepper (capsaicin) may reduce pain by interfering with signals from the joint to the brain. If that fails, physicians can prescribe disease-modifying anti-rheumatic drugs (DMARDs) to stop or slow the immune system from attacking the joints. Biologic response modifiers (Enbrel) may also be used to target specific protein molecules, and corticosteroids (Cortisol) can help suppress the immune system and reduce joint inflammation.
Therapies
Physicians may recommend acupuncture, physical, massage, or talk therapy to help reduce and cope with arthritic pain.
Surgery
For some patients, surgery is a consideration if conservative treatments fail and activities of daily living are significantly disrupted. Joint repair can smooth or realign surfaces, and be performed arthroscopically with minimal invasion. Artificial hips or knees can replace damaged joints, and joint fusions can lock wrists, ankles, and fingers to reduce friction and pain.