Pain
Progression and Complications Spinal Stenosis
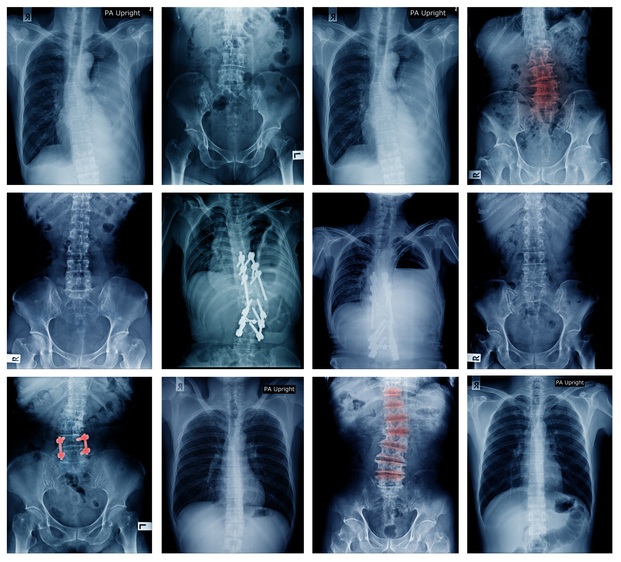
What is spinal stenosis?
Spinal stenosis is a narrowing of the spinal canal. It occurs when the bony openings within the spine (foramina) begin to narrow, placing pressure on the nerves traveling throughout the spine. This reduced nerve space can occur within the spinal cord or where the spinal nerves exit the spinal canal. Spinal stenosis most commonly affects the upper neck (cervical) and lower back (lumbar); however, although rare, the upper and middle back (thoracic) can also be affected.
Progression and complications of spinal stenosis
Although many people with spinal stenosis may need to make physical activity modifications, most lead full and active lives. However, spinal stenosis can lead to the following:
- Slow and steady loss of strength in the legs
- Nerve compression
- Increased pain
- Residual pain after treatment or surgery
Although rare, untreated spinal stenosis can progress and cause life-long complications including the following:
- Balance problems
- Increased risk of falls
- Incontinence
- Numbness
- Paralysis
- Weakness
Associated medical conditions
Medical conditions that may accompany or develop from spinal stenosis:
- Spondylolisthesis is a spinal condition involving the lower vertebra, in which one vertebra slips forward onto the bone beneath it.
- Facet joint syndrome is an arthritic-like condition of the spine. There are two facet joints on each vertebra that link each vertebra together. These facet joints provide support, stability and mobility of the spine. When they break down, they provide less support to the spine, leading to pain, stiffness, and pressure on the nerves of the spinal cord.
- Cauda equina syndrome is a possible complication of spinal stenosis and is a medical emergency. Symptoms include impaired bladder or bowel control, difficulty walking, or paralysis. This requires immediate medical treatment.


















